Hepatobiliary and Pancreatic Unit
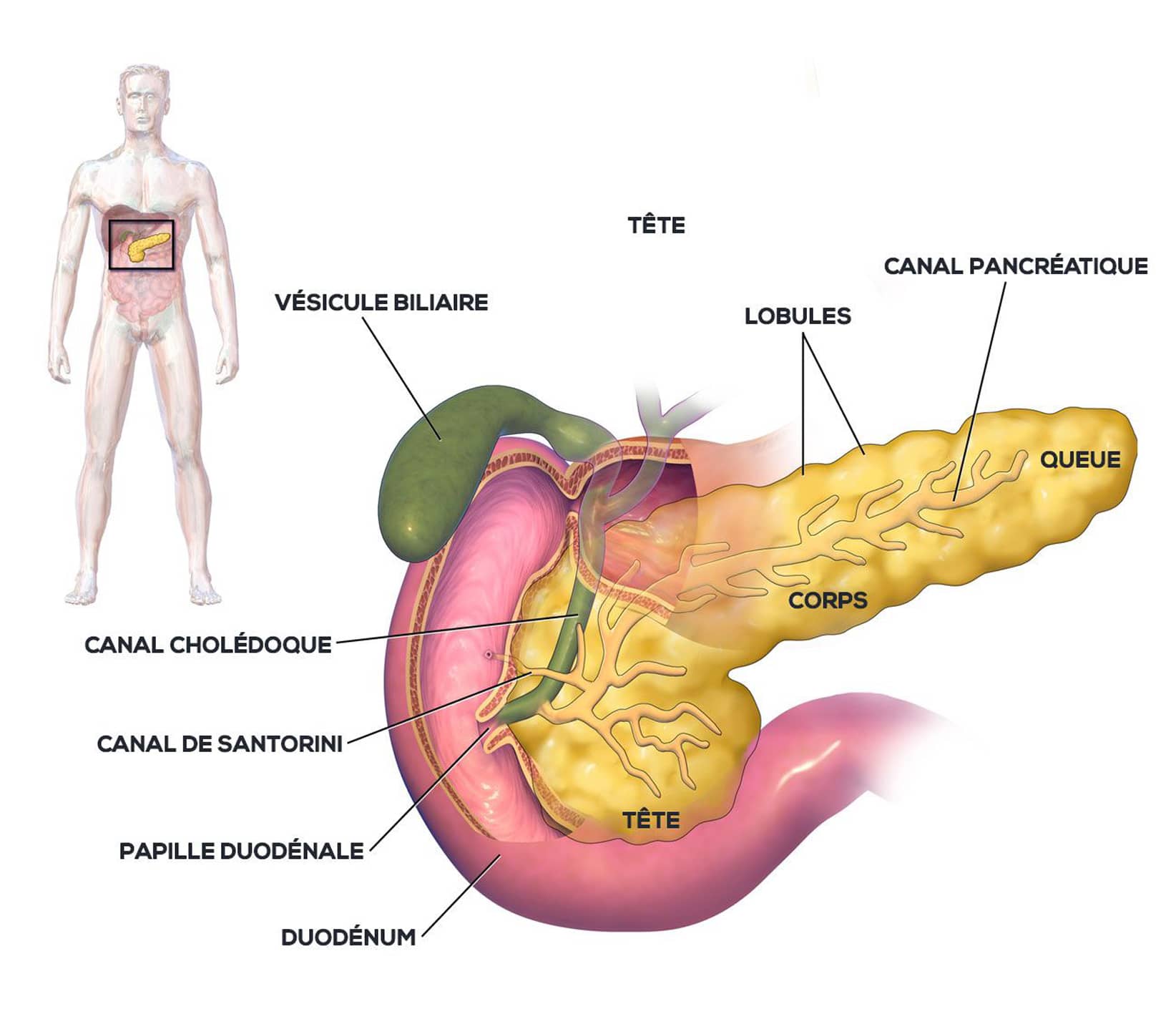
Anatomy of the pancreas
The pancreas is a visceral organ located in the abdomen, in the retroperitoneum, in front of the aorta and inferior vena cava, and behind the stomach. It is a gland of the digestive system.
The pancreas is the second largest gland after the liver.
Pale pink in color, the pancreas is normally soft and granular in appearance. It measures between 12 and 15 cm in adults and weighs approximately 80g. Its thickness decreases from right to left. The pancreas is divided into three parts, from its medial end to its lateral end: the head, the body and the tail.
The pancreas produces enzyme-rich secretions, which are discharged into the duodenum to aid digestion (exocrine function), and hormones, including insulin, which are discharged into the bloodstream to help regulate blood sugar levels (endocrine function).
Pancreatic tumors
When a mass is found in the pancreas, it may be a benign, non-cancerous lesion, or it may be malignant.
The most common malignant tumor is pancreatic ductal adenocarcinoma (90% of cases).
Other, less frequent tumors may be present: neuroendocrine tumors (3% of cases) developed from pancreatic endocrine cells (hormone-producing cells), or cystadenocarcinomas (1-2% of cases).
Pancreatic cancer, or pancreatic adenocarcinoma, is a cancer of the pancreatic gland that secretes digestive enzymes. Worldwide, the incidence varies between 1 and 10 cases per 100,000 people. Pancreatic adenocarcinoma (PA) accounts for 90% of pancreatic tumors; its incidence in France has doubled in men and tripled in women since the 1980s. It remains the digestive cancer with the poorest prognosis, with a 5-year overall survival rate (OS), all stages combined, of 7% to 8%.

Cystic adenocarcinoma of the head of the pancreas, Wikimedia Commons
Risk factors
Several factors can contribute to the development of this cancer:
- smoking
- being overweight or obese
- genetic factors
- pre-existing pancreatic disease, such as chronic pancreatitis
Symptoms
When pancreatic adenocarcinoma is in its early stages, in most cases it is asymptomatic
Symptoms often appear later, when the tumor has developed outside the pancreas.
As the disease progresses, the following signs may appear:
- strong, persistent pain behind the stomach or in the back,
- weight loss,
- fatigue,
- jaundice – an increase in bilirubin levels in the blood and skin,
- itching (pruritus),
- problems with digestion – this can be difficult and painful,
- changes in intestinal transit (diarrhea, nausea, constipation),
and, in some cases, a rise in body temperature with fever.
Other symptoms of cancer can include a marked deterioration in the patient’s general condition, and significant weight loss.
Diagnosis and management
In the case of a lesion in the head of the pancreas (or cephalic lesion), compression of the bile duct passing through the head of the pancreas may be associated with jaundice. A biliary prosthesis may be required to remove the obstruction, thereby reducing bilirubin levels and treating jaundice.
To rule out distant metastases, extension studies may include pancreatic and hepatic MRI, and thoraco-abdomino-pelvic CT scans.
Early diagnosis combined with a rapid extension work-up is essential.
A biopsy of the lesion can be performed under echo-endoscopy to obtain the anatomopathological characteristics of the lesion.
f the patient is malnourished prior to surgery, treatment with nutritional supplements may be considered. If the lesion is unresectable, initial chemotherapy (neoadjuvant) may be considered to reduce the size of the lesion and make it potentially resectable.
Treatment – Post-operative follow-up
Patient cases are discussed at multidisciplinary consultation meetings held once a week at Strasbourg’s NHC (Nouvel Hôpital Civil). The aim of these meetings is to establish the best therapeutic protocol for patients being treated for cancer. This means that the patient’s treatment is not decided by a single doctor, but by a multidisciplinary team of doctors.
Treatment of pancreatic cancer must take into account the cause, course and severity of the pancreatic disease. Therapeutic possibilities will be considered depending on the grade and severity of the disease.
Different therapies can be implemented such as:
- Curative surgery with pancreatic resection of the main tumor. This resection can be considered for the treatment of a tumor that does not exceed a certain volume and which does not present metastases or too close contact with the portal vein and other vessels. This surgery is proposed when all these parameters and the general condition of the patient are optimal. There is currently very little indication for palliative surgery aimed at treating symptoms. Minimally invasive endoscopic or radiological treatments are preferred in these situations.
- This palliative surgery is chosen in the event of failure of minimally invasive approaches in order to allow the flow of bile and the food bolus by carrying out biliary and digestive diversions.
- Neoadjuvant chemotherapy
Chemotherapy can also be offered in cases of advanced disease in order to improve the patient’s quality of life by alleviating the symptoms of the disease and obtaining a reduction in the size of the lesion to make it operable. - Complementary chemotherapy After complete surgery, additional so-called adjuvant chemotherapy is offered to reduce the risk of recurrence.
Useful information
Download guide: Pancreatic cancer treatments
by National Cancer Institute, e-cancer.fr
Cancer Info Line
Support throughout your care pathway
Quality patient care is an essential objective, and the patient is at the heart of our concerns.